COVID-19 Surge, Idaho Activates Crisis Care
Current Visitor Restrictions at Madison Memorial: There can only be one (1) designated visitor per patient, for the length of the patient’s stay (i.e., not one visitor at a time; only one visitor, who may come and go as needed, but is always the same person) No one...

The Daily Special with Heather Metcalf
Story and Photo by Jeremiah Kalb When you think of “Madisonhealth,” what sorts of images pop into your mind? Is it the life-saving measures available in the ER? Maybe the state-of-the-art imaging technology for head-to-toe? Possibly the welcoming of new life at the...

Scuba Diving in Eastern Idaho with Business Intelligence Specialist Kaylynn Yates
Story by Jeremiah Kalb A leading intellectual of his time, Benjamin Franklin, once said, “For the best return on your money, pour your purse into your head.” Business Intelligence Specialist Kaylynn Yates did this when she invested a tiny fortune in scuba gear and...
Holiday Pies, 2022
We’re coming up on that time of year again and Thanksgiving is right around the corner! To make your holiday festivities easier, the Paragon will be offering thaw-and-serve and ready-to-bake pies as well as ready-to-eat rolls. The following pie flavors will be...
Janice Berrett: New Manager of Medical Staff Office
No one is more critical to the success of Madisonhealth than our excellent providers. The Medical Staff Office manager is a key position, one which impacts each of our providers directly. Much time and effort went into the selection process for this vital role, with...
Find My Mojo
Find MY MojoWhat is Find My Mojo? Check out this short overview video to learn more. Sign Up Jeremiah Kalb, HIM Director & Job Crafting Coachof leaders are seeking new jobs post pandemicof workers have an anxiety disorderof workers are disengaged in their...

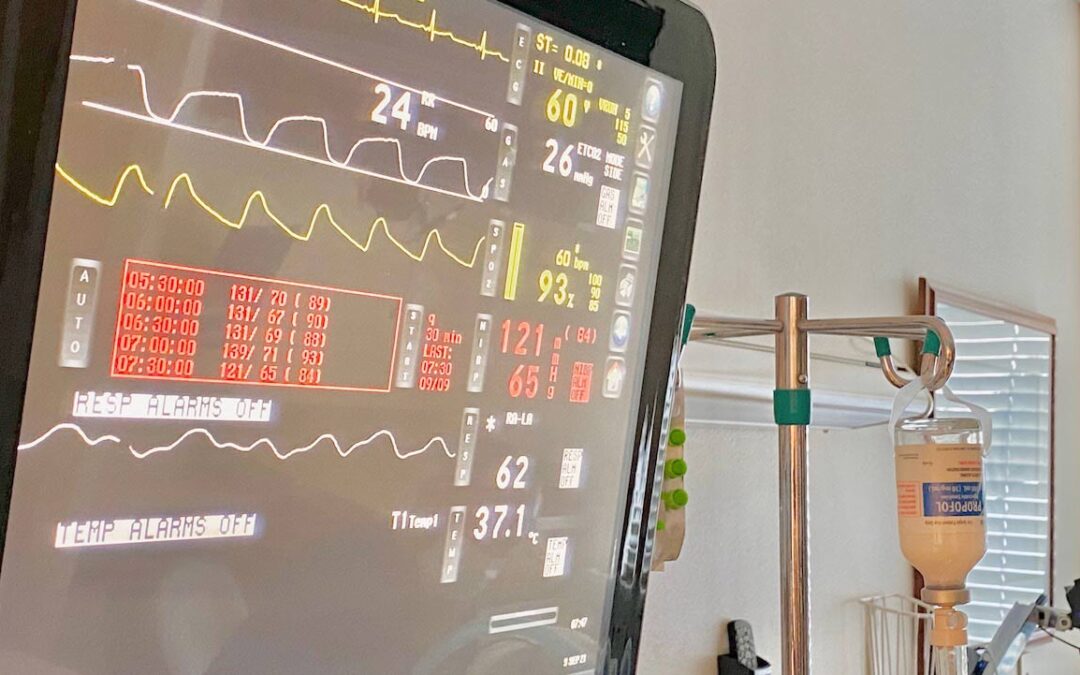
Behind the Scenes of COVID19: Respiratory Therapist Gerod Jones Helps Patients Breathe Easier
Story and Photo by Jeremiah Kalb Once behind-the-scenes health care workers, respiratory therapist Gerod Jones, and his colleagues have garnished worldwide recognition for their expertise on breathing – the issue at the core of the pandemic. Not being able to breathe...
